With just a few hundred cells, scientists have made a ground-breaking discovery in tissue regeneration and personalized medicine.
Researchers and scientists at Tufts University have found a way to fuse tracheal and neural tissue, enabling these cells to transform into robotics. This remarkable breakthrough has the potential to revolutionize the field of medicine and pave the way for exciting new developments in the future.
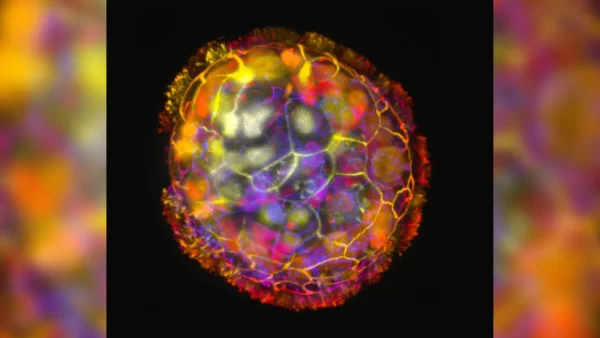
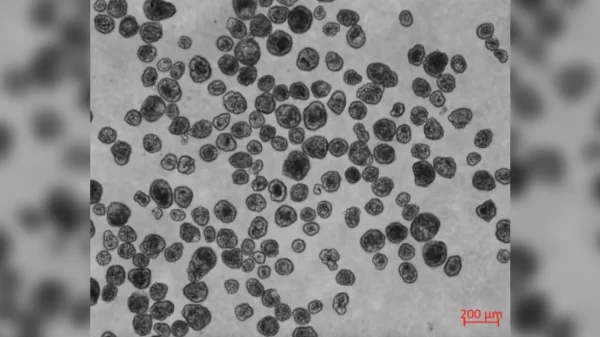
By creating “Anthrobots” or tiny robots made with biological materials, which can range in size from the width of a human hair to the tip of a sharpened pencil, a significant milestone in the field of medicine is marked complete.
A path opens to the new field of tissue regeneration and development. In addition to providing disease treatment and healing, Anthrobot services are specifically tailored to each patient for optimal results.
In research that builds on earlier investigations by Michael Levin and Gizem Gumuskaya, a new study has found that it is possible to create biological robots using adult human cells without any genetic modification.
The previous research had successfully created Xenobots, which were multicellular biological robots from frog embryo cells and were capable of performing various functions such as recording information, replicating cycles on their own, healing themselves from injury and even navigating passageways and collecting material. However, researchers were not sure if these abilities were specific to the amphibian embryo-derived cells or if they could be replicated with cells from other species.
In the current study published in Advanced Science, Levin and Gumuskaya demonstrated that bots constructed from adult human cells have capabilities beyond those observed in the Xenobots. This study also revealed that biological robots can be created using adult human cells without any genetic modification.
“We wanted to probe what cells can do besides create default features in the body,” Gumuskaya said in an interview with Tufts Now. “By reprogramming interactions between cells, new multicellular structures can be created, analogous to the way stone and brick can be arranged into different structural elements like walls, archways or columns.”
Levin and Gumuskaya discovered that the cells could not only generate innovative shapes of multicellular structures but also move in diverse ways over a layer of human neurons cultivated in a laboratory dish.
It was also noticed that the bots were able to stimulate new growth to fill in the gaps caused by scratching the neuronal cell layer. However, the method by which these bots promote neuron growth is yet to be determined. Although researchers verified that neurons grew beneath the area covered by a group of Anthrobots, referred to as a “superbot.”
“The cellular assemblies we construct in the lab can have capabilities that go beyond what they do in the body,” Levin said in an interview with Tufts Now. “It is fascinating and completely unexpected that normal patient tracheal cells, without modifying their DNA, can move on their own and encourage neuron growth across a region of damage.”
In the future, Levin, Gumuskaya and their team believe that Anthrobots created from a patient’s tissue could be utilized to clear arteries, dissolve mucus or administer medications, with or without genetic engineering. No matter which procedure these Anthrobots are used for in the future, the new outlook in medicine seems to only go up from here.